The Takeaway
- Narcolepsy is an important cause of chronic sleepiness, affecting about 1 in 2,000 people. It typically develops during the teen years and lasts for life.
- Narcolepsy is a manageable condition, and people with narcolepsy can lead full and rewarding lives.
Narcolepsy is a neurologic disorder and is one of the most common causes of chronic sleepiness.
-Dr. Thomas Scammell
Narcolepsy is a neurological disorder that causes persistent sleepiness and additional symptoms such as brief episodes of muscle weakness known as cataplexy, vivid, dreamlike hallucinations, brief episodes of paralysis when falling asleep or upon awakening (sleep paralysis), and fragmented nighttime sleep. Symptoms typically develop over several months and last a lifetime.

The disorder usually begins between ages 10 and 20, although sometimes it starts as late as age 40 or 50. Narcolepsy affects women and men equally, occurring in about 1 in 2,000 people.
Narcolepsy is a manageable condition, and with an array of treatment strategies, people with narcolepsy can live full and rewarding lives.
For a one-page summary of narcolepsy and its symptoms, causes, and treatments, download What Is Narcolepsy? (PDF).
Types of narcolepsy
Clinicians now recognize two major types of narcolepsy: narcolepsy with cataplexy (muscle weakness triggered by strong emotions) and narcolepsy without cataplexy. People who have narcolepsy without cataplexy have sleepiness but no emotionally triggered muscle weakness, and generally have less severe symptoms.

There also exists another, very rare type known as secondary narcolepsy, which occurs with injury to a deep part of the brain called the hypothalamus. In addition to any of the typical narcolepsy symptoms, people with secondary narcolepsy also have severe neurological problems and require large amounts (>10 hours) of sleep.
Sleep basics
To understand the symptoms of narcolepsy, it helps to first understand how sleep happens normally. Healthy sleep includes two types of sleep: rapid-eye-movement (REM) sleep and non-REM (NREM) sleep.
REM sleep is characterized by dreams, quick eye movements, and paralysis of the limbs and trunk that prevents someone from acting out dreams and getting injured during sleep. In non-REM sleep, dreams are less common and the body is not paralyzed. In individuals without narcolepsy, REM sleep, non-REM sleep, and wakefulness are distinct states that do not mix together.
To learn more about types of sleep and sleep cycles, see Healthy Sleep.
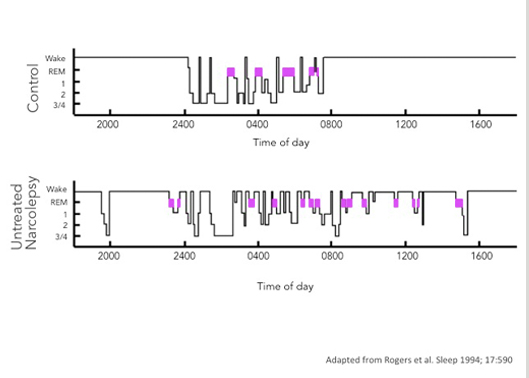
In people with narcolepsy, the regulation of sleep is disrupted: the boundaries between wakefulness and sleep are less distinct, and elements of sleep and wakefulness can mix together.
The sleep patterns of people with narcolepsy differ in several ways from the sleep patterns of people who do not have the disorder:
| People with narcolepsy | People without narcolepsy |
|---|---|
| During the day | |
| Feel drowsy, inattentive, and fall asleep easily | Feel alert, awake, and don’t readily fall asleep |
| Often enter REM sleep and dream during naps | Generally do not enter REM sleep or dream during naps |
| Hallucinations on waking common | Hallucinations on waking uncommon |
| Sleep paralysis common | Sleep paralysis uncommon |
| May experience cataplexy | Never experience cataplexy |
| During the night | |
| Spontaneously wake from sleep | Generally sleep well |
| Can enter REM sleep within 15 minutes | Start out in non-REM sleep and then take 60–90 minutes to enter REM sleep |