
Most people don’t get enough sleep. We are a society that burns the candle at both ends, a nation where people stay up all night to study, work, or have fun. However, going without adequate sleep carries with it both short- and long-term consequences.
In the short term, a lack of adequate sleep can affect judgment, mood, ability to learn and retain information, and may increase the risk of serious accidents and injury. In the long term, chronic sleep deprivation may lead to a host of health problems including obesity, diabetes, cardiovascular disease, and even early mortality.
Sleep and Disease Risk
The Takeaway
- The cost of poor sleep is much greater than many people think: it may have profound consequences for our long-term health.
- Research has revealed that people who consistently fail to get enough sleep are at an increased risk of chronic disease, and scientists are now beginning to understand why.
- Treating sleep as a priority, rather than a luxury, may be an important step in preventing a number of chronic medical conditions.
The Relationship Between Sleep and Health
The price of insufficient sleep may be poor health. Study after study has revealed that people who sleep poorly are at greater risk for a number of diseases and health problems. And now the search is on to discover why this might be.
We all have some sense of the relationship between sleep and our ability to function throughout the day. After all, everyone has experienced the fatigue, bad mood, or lack of focus that so often follow a night of poor sleep. What many people do not realize is that a lack of sleep—especially on a regular basis—is associated with long-term health consequences, including chronic medical conditions like diabetes, high blood pressure, and heart disease, and that these conditions may lead to a shortened life expectancy. Additional research studies show that habitually sleeping more than nine hours is also associated with poor health.
Researching the Link Between Sleep Duration and Chronic Disease
There are three main types of study that help us understand the links between sleep habits and the risk of developing certain diseases. The first type (called sleep deprivation studies) involves depriving healthy research volunteers of sleep and examining any short-term physiological changes that could trigger disease. Such studies have revealed a variety of potentially harmful effects of sleep deprivation usually associated with increased stress, such as increased blood pressure, impaired control of blood glucose, and increased inflammation.
The second type of research (called cross-sectional epidemiological studies) involves examining questionnaires that provide information about habitual sleep duration and the existence of a particular disease or group of diseases in large populations at one point in time. For example, both reduced and increased sleep duration, as reported on questionnaires, are linked with hypertension, diabetes, and obesity. However, cross-sectional studies cannot explain how too little or too much sleep leads to disease because people may have a disease that affects sleep, rather than a sleep habit that causes a disease to occur or worsen.
The third and most convincing type of evidence that long-term sleep habits are associated with the development of numerous diseases comes from tracking the sleep habits and disease patterns over long periods of time in individuals who are initially healthy (i.e., longitudinal epidemiological studies). We do not yet know whether adjusting one’s sleep can reduce the risk of eventually developing a disease or lessen the severity of an ongoing disease. However, the results from longitudinal epidemiological studies are now beginning to suggest that this is likely.
Dr. Orfeu Buxton describes how animal and human studies suggest that adequate sleep is crucial for a long and healthy life.
Below is some of the evidence demonstrating the relationship between sleep habits and risk for developing certain medical conditions.
Obesity
Several studies have linked insufficient sleep and weight gain. For example, studies have shown that people who habitually sleep less than six hours per night are much more likely to have a higher than average body mass index (BMI) and that people who sleep eight hours have the lowest BMI. Sleep is now being seen as a potential risk factor for obesity along with the two most commonly identified risk factors: lack of exercise and overeating. Research into the mechanisms involved in regulating metabolism and appetite are beginning to explain what the connection between sleep and obesity might be.

Insufficient sleep is also associated with lower levels of leptin, a hormone that alerts the brain that it has enough food, as well as higher levels of ghrelin, a biochemical that stimulates appetite. As a result, poor sleep may result in food cravings even after we have eaten an adequate number of calories. We may also be more likely to eat foods such as sweets that satisfy the craving for a quick energy boost. In addition, insufficient sleep may leave us too tired to burn off these extra calories with exercise.
Diabetes
Researchers have found that insufficient sleep may lead to type 2 diabetes by influencing the way the body processes glucose, the high-energy carbohydrate that cells use for fuel. One short-term sleep restriction study found that a group of healthy subjects who had their sleep cut back from 8 to 4 hours per night processed glucose more slowly than they did when they were permitted to sleep 12 hours. Numerous epidemiological studies also have revealed that adults who usually slept less than five hours per night have a greatly increased risk of having or developing diabetes.
In addition, researchers have correlated obstructive sleep apnea—a disorder in which breathing difficulties during sleep lead to frequent arousals—with the development of impaired glucose control similar to that which occurs in diabetes. Explore APNEA
Heart Disease and Hypertension

Studies have found that a single night of inadequate sleep in people who have existing hypertension can cause elevated blood pressure throughout the following day. This effect may begin to explain the correlation between poor sleep and cardiovascular disease and stroke. For example, one study found that sleeping too little (less than six hours) or too much (more than nine hours) increased the risk of coronary heart disease in women.
Dr. Janet Mullington discusses how studies suggest a link between sleep deprivation and increased risk for cardiovascular disease.
There is also growing evidence of a connection between obstructive sleep apnea and heart disease. People who have apnea typically experience multiple awakenings each night as a result of the closing of their airway when they fall asleep. In addition to these sleep disturbances, apnea sufferers also experience brief surges in blood pressure each time they wake up. Over time, this can lead to the chronic elevation of blood pressure known as hypertension, which is a major risk factor for cardiovascular disease. Fortunately, when sleep apnea is treated, blood pressure may go down.
Mood Disorders
Given that a single sleepless night can cause people to be irritable and moody the following day, it is conceivable that chronic insufficient sleep may lead to long-term mood disorders. Chronic sleep issues have been correlated with depression, anxiety, and mental distress. In one study, subjects who slept four and a half hours per night reported feeling more stressed, sad, angry, and mentally exhausted. In another study, subjects who slept four hours per night showed declining levels of optimism and sociability as a function of days of inadequate sleep. All of these self-reported symptoms improved dramatically when subjects returned to a normal sleep schedule.
Immune Function
It is natural for people to go to bed when they are sick. Substances produced by the immune system to help fight infection also cause fatigue. One theory proposes that the immune system evolved "sleepiness inducing factors" because inactivity and sleep provided an advantage: those who slept more when faced with an infection were better able to fight that infection than those who slept less. In fact, research in animals suggests that those animals who obtain more deep sleep following experimental challenge by microbial infection have a better chance of survival.
Alcohol

Studies have shown that alcohol use is more prevalent among people who sleep poorly. The reason for this is twofold. First, alcohol acts as a mild sedative and is commonly used as a sleep aid among people who have sleep problems such as insomnia. Second, the sedative quality of alcohol is only temporary. As alcohol is processed by the body over a few hours it begins to stimulate the parts of the brain that cause arousal, in many cases causing awakenings and sleep problems later in the night.
Life Expectancy
Considering the many potential adverse health effects of insufficient sleep, it is not surprising that poor sleep is associated with lower life expectancy. Data from three large cross-sectional epidemiological studies reveal that sleeping five hours or less per night increased mortality risk from all causes by roughly 15 percent.
Of course, just as sleep problems can affect disease risk, several diseases and disorders can also affect the amount of sleep we get. While an estimated 50 to 70 million Americans suffer from some type of sleep disorder, most people do not mention their sleeping problems to their doctors, and most doctors do not necessarily ask about them. This widespread lack of awareness of the impact of sleep problems can have serious and costly public health consequences.
To learn more about sleep disorders, the risks they pose, and possible treatment options, see An Overview of Sleep Disorders.
References
- Sigurdson K, Ayas N. The public health and safety consequences of sleep disorders. Can J Physiol Pharmacol. 2007; 85:179-83
- Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007; 30:1245-53.
- Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB. A prospective study of sleep duration and mortality risk in women. Sleep. 2004; 27:440-4.
Sleep, Performance and Public Safety
The Takeaway
- The demands and expectations of our modern society have placed increasing demands on our time, and more than ever people are making up for those demands by cutting back on sleep.
- At the same time, it is becoming increasingly clear that the cost of insufficient sleep is much higher than most people recognize.
- Scientific research is revealing, for example, how sleep loss, and even poor-quality sleep, can lead to an increase in errors at the workplace, decreased productivity, and accidents that cost both lives and resources. Awareness can help you improve your sleep habits and in turn your safety.
Costly, Preventable Accidents

Insufficient sleep may not have led the news in reporting on serious accidents in recent decades. However, that doesn't mean fatigue and inattention due to sleep loss didn't play a role in these disasters. For example, investigators have ruled that sleep deprivation was a significant factor in the 1979 nuclear accident at Three Mile Island, as well as the 1986 nuclear meltdown at Chernobyl.
Investigations of the grounding of the Exxon Valdez oil tanker, as well as the explosion of the space shuttle Challenger, have concluded that sleep deprivation also played a critical role in these accidents. In both cases, those in charge of the operations and required to make critical decisions were operating under extreme sleep deprivation. While the Challenger disaster put the multi-billion dollar shuttle program in peril, the Exxon Valdez oil spill resulted in incalculable ecological, environmental, and economic damage.
Dr. Robert Stickgold discusses a study that suggests a link between sleep loss and impaired judgement.
In addition to the ties between such high-profile disasters and sleep deprivation, there is a growing recognition of the link between lack of sleep and medical errors in our hospitals. According to the Institutes of Medicine, over one million injuries and between 50,000 and 100,000 deaths each year result from preventable medical errors, and many of these may be the result of insufficient sleep, Doctors, especially newly graduated interns, are often expected to work continuous shifts of 24 to 36 hours with little or no opportunity for sleep.
Although it is difficult to estimate the extent that sleep deprivation plays in medical errors, studies have shown a significant impact. For example, a 2004 study led by Dr. Charles Czeisler of the Division of Sleep Medicine at Harvard Medical School found that hospitals could reduce the number of medical errors by as much as 36 percent by limiting an individual doctor’s work shifts to 16 hours and reducing the total work schedule to no more than 80 hours per week.
Long shifts and other factors that result in sleep loss have safety consequences for our highways as well. A National Sleep Foundation survey has revealed that 60 percent of adult drivers—about 168 million people—say they have driven a vehicle while feeling drowsy in the past year, and that more than one-third (103 million people) have actually fallen asleep at the wheel. Unfortunately, many of these situations end in tragedy. The National Highway Traffic Safety Administration estimates that 100,000 police-reported crashes are the direct result of driver fatigue each year, and they consider this a conservative estimate. More recent data suggests that the true number is likely much higher. The Institute of Medicine estimates—based on recent high quality naturalistic and epidemiologic studies—that drowsy driving is responsible for fully 20 percent of all motor vehicle crashes. That would mean that drowsy driving causes approximately 1 million crashes, 500,000 injuries, and 8,000 deaths each year in the U.S.
Dr. Charles Czeisler discusses the link between motor vehicle accidents and tired drivers.
How Sleep Deprivation Affects Mental Performance

The earliest scientific evidence of a link between sleep and performance dates back to the early 1930’s, when Nathaniel Kleitman, one of most significant figures in the field of sleep medicine, discovered a daily pattern in the speed and accuracy of cognitive performance. He showed that even in well-rested individuals there was a decrease in the level of individual performance that occurred in the early morning and again late at night. Thus, even when we are getting the amount of sleep we need, we can still expect normal fluctuations in our ability to function.
In addition to these normal fluctuations, not getting enough sleep—whether for just one night or over the course of weeks to months—has a significant effect on our ability to function. Sleep deprivation negatively impacts our mood, our ability to focus, and our ability to access higher-level cognitive functions. The combination of these factors is what we generally refer to as mental performance. In the laboratory, researchers use scientific studies to determine just how significantly varying levels of sleep disturbance impact various types of mental performance.
Dr. Charles Czeisler describes four factors that affect alertness and performance.
The most immediate effect of sleep deprivation is sleepiness. In our daily lives, we may experience this as a general fatigue, lack of motivation, or even the experience of nodding off. In the research or clinical setting, scientists measure sleepiness using a variety of methods. After a period of sleep deprivation, there are noticeable changes in brain activity, as measured by an electroencephalogram (EEG). These changes correspond to a lower level of alertness and a general propensity to sleep. Any period of continual wakefulness beyond the typical 16 hours or so will generally lead to these measurable changes.
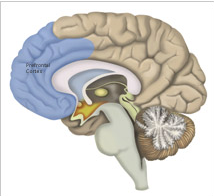
In addition to the feeling of sleepiness and changes in brain activity that accompany a night without sleep, other measures of performance are noticeably altered. Concentration, working memory, mathematical capacity, and logical reasoning are all aspects of cognitive function compromised by sleep deprivation. However, not all of these functions rely on the same regions of the brain, nor are they impacted by sleep deprivation to the same degree. For example, the region of the brain known as the prefrontal cortex (PFC) is responsible for many higher-level cognitive functions and is particularly vulnerable to a lack of sleep. As a result, people who are sleep deprived will begin to show deficits in many tasks that require logical reasoning or complex thought.
Determining just how much performance is affected by sleep loss is difficult, in part because of factors such as individual differences in sensitivity to sleep deprivation, as well as individual differences in motivation to stay alert despite sleep loss. Even so, the evidence is clear that a lack of sleep leads to poor performance. As the prevalence of inadequate sleep grows and the demands of the workplace change, it becomes increasingly critical that we recognize and take action to mitigate the impact that insufficient sleep has on our safety and well-being.
References
- Harrison Y, Horne J. J Exp Psychol. 2000; 6:236-49
- Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA. N Engl J Med. 2004; 351:1838-48