Normally, when you breathe in, air flows through the nose and/or mouth, past the back of the throat, and down into the lungs (see Figure 1). The reverse occurs when breathing out; the flow goes from the lungs through the throat, and then out the nose and/or mouth. When you fall asleep, breathing remains more or less the same, except that the rate of breathing slows down slightly.
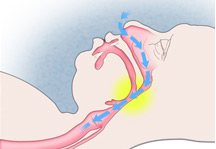
Figure 1: Viewing the head and neck from the side, the blue arrows indicate that during normal inhalation, air flows into the upper airway (pink) through the nose as well as through the mouth (not shown by arrows), down behind the tongue and through the back of the throat (area shown in yellow) into the lungs. During exhalation, the pattern of airflow is reversed. © Image courtesy of New England Journal of Medicine
Obstructive sleep apnea (OSA) occurs when a person' airway repeatedly becomes blocked despite efforts to breathe (see Figure 2). This breathing cessation is called obstructive sleep apnea. In cases where there are frequent episodes of both complete and partial blockage, the term obstructive sleep apnea hypopnea is used.

Figure 2: Obstruction of the Airway During Apnea. Viewing the head and neck from the side, the airway (pink) is blocked by the tongue falling back against the back of the throat (area shown in yellow). No airflow can occur. © Image courtesy of New England Journal of Medicine
What happens during an apnea?
To understand what is going on in an apnea, it's helpful to think of this analogy. Imagine trying to drink a milkshake through a paper soda straw. As you suck in, the weak paper straw collapses, and you don't get any of the milkshake. This collapsing is similar to what happens to people with OSA, but instead of missing out on a milkshake, they don't get enough air into their lungs. This does not occur with normal breathing during wakefulness because signals from the brain activate the tongue and the muscles surrounding the airway and stiffen the airway. Therefore, air can flow into the lungs uninterrupted. In other words, normal breathing during wakefulness is like drinking the milkshake through a plastic soda straw.
When we sleep, there is an increased risk for the airway behind the tongue to collapse with each breath (particularly when sleeping on our backs). For most people this collapse does not occur because activation of the muscles surrounding the airway during sleep is still strong enough to prevent any blockage. However, for someone with OSA, the muscles do not respond adequately. Like the paper straw that collapses, the airway collapses and air does not reach the lungs.
What happens when the airway is blocked or partially blocked?
When sufficient air doesn't get into a person's lungs, the level of oxygen in the blood falls and the level of carbon dioxide (a waste product of metabolism) rises. After a few minutes of not breathing, a person may die. Fortunately, with OSA, after a period of not breathing, the brain wakes up, and breathing resumes. This period of time can range from a few seconds to over a minute. When breathing resumes, the size of the airway remains reduced in size. The tissues surrounding this narrow airway vibrate—what we call snoring. In other words, snoring is a sign of an obstructed airway, but it does mean that a person is breathing; silence might indicate that the airway is completely blocked.

What are the effects of apnea?
Because waking up is necessary to end an episode of apnea or hypopnea, a person with OSA wakes up again and again throughout sleep. This reduces the duration and quality of sleep. In most cases, a person with OSA is not aware of these repeated awakenings because they occur below the level of consciousness. As a result, people with OSA frequently complain of daytime sleepiness, fatigue, and/or insomnia. This poor sleep may also cause problems with memory, concentration, and mood changes.
There are other physical effects of apnea. In people with OSA, repeated episodes of falling oxygen levels lead to a variety of physiological changes that affect the heart and blood vessels. During these episodes, the heart is stressed, which increases blood pressure and heart rate. There is increased secretion of hormones and substances that are released with stress as well as increased production of compounds that produce inflammation.