The Takeaway
Surgical treatments for obstructive sleep apnea are less common than nonsurgical treatments. Limited success rates, risk levels, and recovery time should be well understood when considering surgical treatment.
Nasal Surgery
In general, operations performed to increase airflow through the nose, such as removal of nasal polyps or turbinates, or straightening a deviated nasal septum, do not completely cure obstructive sleep apnea (OSA) but may improve daytime and nighttime breathing through the nose and may enable better use of positive airway pressure.
Upper Airway Surgery
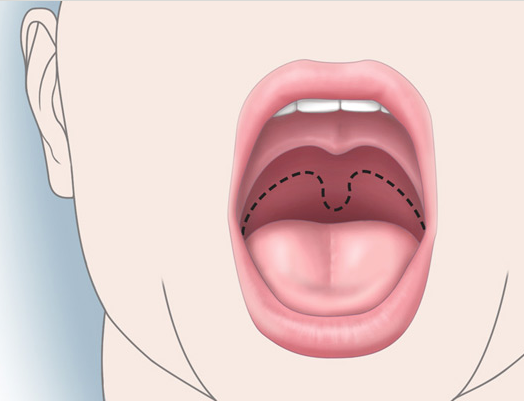
The most common operation performed is called a uvulopalatopharyngoplasty (UPPP). This operation attempts to widen the airway behind the tongue by removing excess tissue from the sides of the throat behind the tongue, shortening the soft palate, and removing the uvula (see Figure 9). The operation requires hospitalization and recovery may take several weeks. Variants of the operation can be performed on an outpatient basis with a laser (laser-assisted uvulopharyngoplasty, or LAUP) or by a radiofrequency probe (somnoplasty). Although snoring is frequently improved with these operations, only approximately 40% of persons undergoing UPPP have resolution or major improvement in their OSA. Furthermore, it is unclear whether the success rates from LAUP or somnoplasty are comparable to those for UPPP. Reported side effects from these operations include changes in voice and difficulty swallowing liquids.
Maxillomandibular Advancement (MMA)
the airway.2
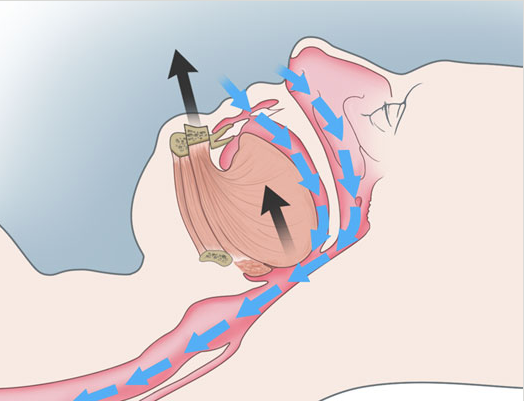
In this operation, the upper and lower jaws are surgically fractured, and both are moved forward to enlarge the airway (see Figure 10). The published results on this operation are reported from only a few institutions, but their results suggest that the improvement rate is greater than for UPPP. However, the operation is substantially more complex than UPPP, with greater risk to the patient and a much longer recovery period.
Tracheostomy
A tracheostomy is a surgically created opening in the trachea below the level of the larynx, or voice box. This bypasses the area of obstruction in OSA. Individuals with a tracheostomy for OSA plug the opening during the day, allowing them to speak normally, but remove the plug for sleep. Tracheostomy was the primary treatment for severe OSA before the introduction of PAP therapy. It is still used for very severe cases that cannot be treated otherwise.
Hypoglossal Nerve Stimulation
In this procedure, a stimulation electrode is surgically placed on branches of the hypoglossal nerve and a sensing electrode is surgically placed in the chest wall. Both are then connected to a neurostimulator which is located in a surgically created pocket just underneath the clavicle. The sensing electrode determines when breathing starts and sends a signal to the neurostimulator. The stimulation electrode then activates the hypoglossal nerve which controls movement of the tongue. When activated, it causes the tongue to move forward. In the setting of obstructive sleep apnea, this will prevent the tongue from collapsing backward thereby preventing obstruction of the upper airway. In recent clinical trials, this procedure has been shown to be successful in treating some patients with obstructive sleep apnea.
Other Procedures
Several other operations have been performed for OSA. These include radiofrequency reduction of the size of the tongue, stiffening the soft palate with stents, advancement of the front of the lower jaw, and relocation of the hyoid bone. None of these operations has been shown to have a high rate of success in the treatment of OSA. However, they may be of benefit in selected cases.
1 Looking into the mouth toward the back of the throat, the dotted black line shows the original position of the roof of the mouth. The tissue between the dotted line and roof of the mouth as shown would be removed during a UPPP.
2As viewed from the side, the top black arrow shows the lower jaw being moved forward as a result of surgery, thus pulling the tongue (lower black arrow) forward as well. This decreases the likelihood of the tongue falling back against the back of the throat to block the airway (in pink). The blue arrows indicate unimpeded airflow into the lungs.