Program in Sleep Medicine Epidemiology (SME)
Division of Sleep Medicine, Brigham and Women's Hospital
Director: Susan Redline, MD, MPH
The Program in Sleep Medicine Epidemiology (SME) is uniquely structured to support innovative research aimed at elucidating individual and population-level risk factors for sleep disorders, and to use this knowledge to design and test interventions to improve sleep health. Goals are to: elucidate the role of genetics, early life developmental factors, and environmental exposures on sleep health; identify how social and environmental factors shape sleep health disparities which in turn drive chronic health disparities; and identify the role of sleep interventions in improving health, including cardiovascular, metabolic, and cognitive disorders.
To meet its objectives, faculty in SME lead and conduct:
- large-scale observational research and data analyses that integrate information on physiological, environmental and genomic risk factors;
- rigorous clinical trials to identify the best treatment options for management of sleep disorders;
- comparative effectiveness and patient-centered research, including those addressing sleep health disparities.
The Program in SME is committed to rigorous and transdisciplinary research, training new generations of investigators and clinicians, engaging multiple stakeholders in research, and sharing data to address reproducibility and promote discovery.
The SME developed and supports the following Resources:
- The BWH Sleep Reading Center is an international core laboratory that provides leadership in the design and implementation of sleep data collection for numerous clinical trials and cohort studies. Representative studies it has supported include: Hispanic Community Health Study/Study of Latinos, Jackson Heart Study, MrOS Sleep Study, Multi-Ethnic Study of Atherosclerosis, Nulliparous Pregnancy Outcomes Study, and Sleep Heart Health Study. It spearheaded efforts at establishing rigorous quality control procedures for multi-site sleep research. In collaboration with the Wellman/Sands lab (web site) and Purcell lab, it integrates advanced signal processing analytics into large scale-epidemiological datasets to provide quantitative biomarkers of sleep and sleep disorders.
- The National Sleep Research Resource (NSRR), a NHLBI-data and tool resource repository and community engagement resource designed to share the wealth of research data generated by the BWH Sleep Reading Center and from other investigators with the greater scientific community. It houses polysomnography, actigraphy and other data that have been carefully curated. It leads the development of tools to structure, harmonize, visualize and analyze sleep data.
- The Sleep Apnea Patient-Centered Outcomes Network (MyApnea), a web-based portal to promote sleep apnea patient support and engagement in research.
- The Sleep Innovate platform, a portal to support a virtual sleep disorders patient-cohort, designed as a foundation for precision sleep medicine.
This distinctively organized program merges expertise in Sleep Medicine, epidemiology, genetics, informatics, biomedical engineering, implementation science, and clinical trials.
Members lead the following Cores:
Bioinformatics Core, directed by Brian Cade, Ph.D.
The Bioinformatics core designs solutions for computationally intensive “big data” analyses of sleep and integrates bioinformatics data into improved genetic analyses of normal and disordered sleep. Current areas of focus include electronic health record and natural language processing of hundreds of thousands of patients and terabyte-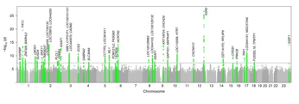 scale whole-genome sequence analyses. Areas of expertise include cluster and cloud computing in a Linux environment, Python and BASH scripting solutions, and database design.
scale whole-genome sequence analyses. Areas of expertise include cluster and cloud computing in a Linux environment, Python and BASH scripting solutions, and database design.
Biostatistics and Genomics Core, directed by Tamar Sofer, Ph.D.
The Biostatistics and Genomics core carries out research in (1) the genetic basis of sleep, (2) its omics-related associations (e.g. metabolomics and DNA methylation patterns associated with sleep phenotypes), (3) statistical methods that address the unique challenges posed by sleep data, which are high dimensional and often have non-normal distributions. In addition, the core provides guidance and expertise in statistical and statistical genetic analysis to the Program in Sleep Medicine Epidemiology.
Data Management Core, led by Michael Rueschman, M.P.H.
This Core supports the databases and web portals for large scale multicenter studies and cross-cohort genetic studies, maintaining thorough documentation of the software and the deployment architecture. It has extensive experience with supporting  activities related to rigorous quality control for a very wide variety of data acquisition and analyses operations and implements specialized procedures for tracking, integrating, and annotating complex sleep data such as from CPAP devices and polysomnograms, and implements customized procedures for project management for complex studies to ensure protocol adherence, to closely monitor and support recruitment and retention, and to maximize adherence to study interventions, and to ensure that polysomnography is conducted per protocol.
activities related to rigorous quality control for a very wide variety of data acquisition and analyses operations and implements specialized procedures for tracking, integrating, and annotating complex sleep data such as from CPAP devices and polysomnograms, and implements customized procedures for project management for complex studies to ensure protocol adherence, to closely monitor and support recruitment and retention, and to maximize adherence to study interventions, and to ensure that polysomnography is conducted per protocol.
Implementation Science, Behavioral Sleep Medicine Core, directed by Suzanne Bertisch, MD, MS.
This core focuses on behavioral sleep interventions for patients with sleep disorders as well as at-risk communities. Work is grounded in behavioral theory and use of qualitative, quantitative, and implementation science methods to develop, adapt, and test behavioral sleep interventions sleep to improve access and uptake of these interventions to improve sleep health. Collaboration include researchers at the Harvard TH Chan School of Public Health, the Dana Farber Cancer Institute, Harvard Catalyst, as well as several community-based clinics, patient and professional organizations, and patient stakeholder groups.
Neurophysiological Signal Processing Core, directed by Michael J. Prerau, Ph.D.
The Neurophysiological Signal Processing Core provides guidance to investigators to the most appropriate quantitative methods, tools, and resources for processing and analyzing the sleep electroencephalogram and other related signals within their projects. Additionally, the core seeks to promote and disseminate the state-of-the-art in new methods and provide education in best practices for neural data analysis through a series of seminars and tutorials, to be shared with the greater Harvard community and beyond.
Collaborative Programs
Program in Sleep, Psychiatry, and Genetics, directed by Shaun Purcell, Ph.D.
The Program in Sleep, Psychiatry, and Genetics is a joint program between the Brigham and Women’s Hospital (BWH) Department of Psychiatry and Department of Medicine (Division of Sleep and Circadian Disorders). Through collaborative research, Dr. Purcell and members of the National Sleep Research Resource team develop methods for extracting multiple features from the sleep EEG (and other physiological signals) and make robust tools available to the user community.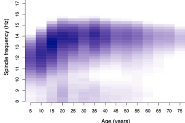
Active Clinical Trials
- Down Syndrome and Sleep Apnea trial (dosatrial.org)
- A hybrid effectiveness-implementation trial evaluating behavioral treatments for insomnia for socioeconomically disadvantaged adults in primary care
Active Cohort Studies/Sleep Reading Center Studies
- Multi-ethnic Study of Atherosclerosis (MESA)
- Hispanic Community Health Study/Study of Latinos (HCHS/SOL; SANAR)
- RECOVER (Researching COVID to Enhance Recovery)
- CRIC (Sleep-disordered breathing as a predictor of outcomes in chronic kidney disease)
- Environmental Assessment of Sleep in Youth
- Hable-Domir (Sleep Quality and Mechanistic Links to Alzheimer's Disease and Related Disorders among older Mexican Americans and Non-Hispanic Whites)
- POINTERZzz (PrOtect through a lifestyle INTErvention to Reduce risk)
- PRISM (Influence of prenatal air pollutant and stress exposures on sleep outcomes in urban preschool-aged children)
- SONNET (Linking Sleep Disruption to Neuronal Dysfunction and Tau Accumulation in Early Alzheimer’s Disease)
- MFMU Sleep Pregnancy Intervention Trial
Faculty
- Suzanne Bertisch, M.D., M.P.H.
- Brian Cade, Ph.D.
- Daniel Gottlieb, M.D., M.S.
- Michael Prerau, Ph.D.
- Susan Redline, M.D., M.P.H.
- Tamar Sofer, Ph.D.
- Heming Wang, Ph.D.
Affiliated Faculty
- Ali Azarbarzin, PhD
- Jessie Bakker, PhD
- Tianyi Huang, PhD
- Shaun Purcell, Ph.D.
- Scott Sands, Ph.D.
- Richa Saxena, Ph.D.
- Rui Wang, Ph.D.
- D Andrew Wellman, M.D., Ph.D.
Post-Doctoral Fellows
- Joon Chung, Ph.D.
- Tariq Faquih, Ph.D.
- Seyni-Gueye-Ndiaye, MD
- Matthew Goodman, Ph.D.
- Kaitlin Potts, Ph.D.
- Danielle Wallace, Ph.D
Staff
- Daniel Mobley, RPSGT, CCSH - Program Manager; Sleep Reading Center Director
- Michael Rueschman, MPH - Data Management Director
- Raichel Alex, Ph.D. - Data Scientist
- Jean Arnold, BS, RPSGT – Polysomnologist
- Cecilia Castro, MD, Ph.D.- Epidemiologist
- Qiyun Chen, MS- Research Data Manager
- Carolina Dos Santos, BA - Research Assistant
- Olivia Claflin, BS - Research Assistant
- Emily Kaplan, BS - Senior Research Assistant
- Nuzululu Kurniansyah, MS - Bioinformatician
- Caroline Li, Research Data Manager
- Jared Mahalabi - Student Research Assistant
- Stephanie Marvin, BA, RPSGT - Polysomnologist
- Michael Morrical, RPSGT -Senior Research Assistant
- Pavithra Nagarajan, MS-Bioinformatician
- Oltion Sina, MD- Clinical Trials Manager
- Paige Sparks, BA - Clinical Research Manager
- Brian Spitzer, Ph.D.- Bioinformatician
- Michelle Sterkel, BS, RPSGT - Polysomnologist
- Susan Surovec, BA - Senior Technical Research Assistant
- Meg Tully, MS- Biostatistician
- Juli Ulanski, BS - Polysomnologist
- Ying Zhang, Ph.D. - Data Scientist